Baytown, TX (281) 837-8371

The Definition of Tarsal Tunnel Syndrome

Tarsal tunnel syndrome is a relatively lesser-known condition compared to other nerve-related disorders, yet it can cause significant discomfort and affect daily life. This syndrome occurs when the tibial nerve, which runs along the inside of the ankle, becomes compressed or squeezed as it passes through the tarsal tunnel, which is a narrow space formed by bone and ligaments on the inner side of the ankle. One important fact about tarsal tunnel syndrome is that it shares similarities with carpal tunnel syndrome, a condition affecting the wrist. Individuals with tarsal tunnel syndrome may experience symptoms such as numbness, tingling, burning pain, or electric shock-like sensations in the ankle, heel, and sole of the foot. Various factors, including injury, inflammation, flat feet, or systemic conditions like diabetes, can contribute to the development of this syndrome. If you are experiencing pain in this part of your foot, it is suggested that you visit a podiatrist who can diagnose and treat tarsal tunnel syndrome.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact Abeer M. Foteh, DPM of Greater Houston Foot Centers. Our doctor can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and ankle become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact our office located in Baytown, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome is a condition in which there is a compression of the posterior tibial nerve. The posterior tibial nerve runs along the inside of the ankle into the foot. Tarsal tunnel syndrome is named for the tarsal tunnel, which is a thin space along the inside of the ankle beside the ankle bones. This space contains various nerves, arteries, and tendons, and includes the posterior tibial nerve. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome the tibial nerve is compressed, causing tingling or burning, numbness, and pain.
Common causes of tarsal tunnel syndrome involve pressure or an injury. Injuries that produce inflammation and swelling in or around the tunnel may place pressure on the posterior tibial nerve. Direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or trauma to the tibial nerve, can result in tarsal tunnel syndrome. Diseases that damage nerves, such as diabetes or arthritis, may cause tarsal tunnel syndrome. Those with flat feet are at risk for developing the condition, as the extra pressure and strain placed on the foot may compress the posterior tibial nerve.
Feeling different sensations in the foot at different times is a common symptom of tarsal tunnel syndrome. An afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg. Symptoms are primarily felt on bottom of the foot and/or the inside of the ankle. Symptoms can appear suddenly and may occur due to overuse of the foot.
To diagnose tarsal tunnel syndrome, your podiatrist may examine the foot and tap the posterior tibial nerve to see if symptoms surface. He or she may also order an MRI to determine if a mass is present.
Treating tarsal tunnel syndrome will depend on the decision of your podiatrist. Multiple options are available, however, and can include rest, ice, immobilization, oral medications such as anti-inflammatory drugs (NSAIDS), physical therapy, injection therapy, orthotics, supportive shoes, braces, and surgery.
Ingrown Toenails and Why They Occur

Ingrown toenails occur when the edge of a toenail grows into the surrounding skin, leading to pain, swelling, and redness. This condition typically affects the big toe and can result from various factors, such as improper trimming, wearing tight-fitting shoes, injury, or genetic predisposition. Symptoms include tenderness along the nail border, inflammation, and sometimes infection, which may result in pus or drainage. People with curved or thickened nails, athletes, individuals with poor foot hygiene, or those with certain medical conditions like diabetes are more susceptible to ingrown toenails. Treatment from a podiatrist often involves gently lifting the ingrown edge, trimming the nail properly, and providing guidance on proper nail care techniques. In some cases, a portion of the nail may need to be removed to prevent recurrence. For severe or recurrent ingrown toenails, surgical procedures like partial nail avulsion may be recommended by a podiatrist to alleviate pain and prevent complications. If you have an ingrown toenail, it is suggested that you schedule an appointment with a podiatrist for treatment that is best for your condition.
Ingrown toenails may initially present themselves as a minor discomfort, but they may progress into an infection in the skin without proper treatment. For more information about ingrown toenails, contact Abeer M. Foteh, DPM of Greater Houston Foot Centers. Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails are caused when the corner or side of a toenail grows into the soft flesh surrounding it. They often result in redness, swelling, pain, and in some cases, infection. This condition typically affects the big toe and may recur if it is not treated properly.
Causes
- Improper toenail trimming
- Genetics
- Improper shoe fitting
- Injury from pedicures or nail picking
- Abnormal gait
- Poor hygiene
You are more likely to develop an ingrown toenail if you are obese, have diabetes, arthritis, or have any fungal infection in your nails. Additionally, people who have foot or toe deformities are at a higher risk of developing an ingrown toenail.
Symptoms
Some symptoms of ingrown toenails are redness, swelling, and pain. In rare cases, there may be a yellowish drainage coming from the nail.
Treatment
Ignoring an ingrown toenail can have serious complications. Infections of the nail border can progress to a deeper soft-tissue infection, which can then turn into a bone infection. You should always speak with your podiatrist if you suspect you have an ingrown toenail, especially if you have diabetes or poor circulation.
If you have any questions, please feel free to contact our office located in Baytown, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ingrown Toenails
An ingrown toenail is a nail that has curved downward and grown into the skin. This typically occurs at either the nail borders or the sides of the nail. As a result, pain, redness, swelling, and warmth may occur in the toe. If a break in the skin forms due to the ingrown nail, bacteria may enter and cause an infection in the area; this is typically characterized by a foul odor and drainage.
Ingrown toenails have multiple reasons for developing. In many instances, the condition is a result of genetics and is inherited. The most common cause, however, is improper trimming; cutting the toenails too short forces the skin beside the nail to fold over. An ingrown toenail can also develop due to trauma, such as stubbing the toe, having an object fall on the toe, or participating in activities that involve repeated kicking or running. Wearing shoes that are too tight or too short can also cause ingrown toenails.
Treatment for an ingrown toenail varies between patients and the severity of the condition. In most cases, it is best to see your podiatrist for thorough and proper treatment. After examining your toe, your podiatrist may prescribe oral antibiotics to clear the infection if one is present. Surgical removal of either a portion of the nail or the entire nail may also be considered. In some cases, complete removal or destruction of the nail root may be required. Most patients who undergo nail surgery experience minimal pain afterward and can return to normal activity the following day.
Ingrown toenails can be prevented with proper nail trimming and by avoiding improper-fitting shoes. When cutting the toenails, be sure that you are cutting in a straight line and avoid cutting them too short. Shoes should not be too short or tight in the toe box.
The Podiatrist's Role in Diabetic Foot Care

Foot care is a critical aspect of diabetic management, as individuals with diabetes are prone to foot comp-lications. Maintaining skin integrity is essential, especially in diabetic feet where issues like neuropathy and poor circulation can lead to ulcers, infections, and possibly even amputations. Preventive care and regular screening are paramount in mitigating risks. A multidisciplinary team, including podiatrists, plays a pivotal role in diabetic foot care. Podiatrists specialize in assessing foot health, identifying early signs of complications, and providing tailored interventions. They offer expertise in wound care, orthotic management, and footwear recommendations, all aimed at preventing and managing foot problems. By emphasizing preventive measures, such as daily foot inspections, proper hygiene, and appropriate footwear, podiatrists collaborate with patients to minimize the likelihood of diabetic foot complications. If you are a diabetic patient, it is strongly suggested that you schedule regular appointments with a podiatrist as part of your diabetes management.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Abeer M. Foteh, DPM from Greater Houston Foot Centers. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Baytown, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Heel Pain While Walking

Heel pain stemming from walking can arise from various underlying conditions, including plantar fasciitis, fat pad atrophy, arthritis, and Achilles tendonitis. Plantar fasciitis involves inflammation of the plantar fascia, the tissue connecting the heel to the toes. This condition commonly causes sharp pain upon initial steps in the morning. Fat pad atrophy results in decreased cushioning under the heel, leading to discomfort with weight-bearing activities. Arthritis may cause stiffness and pain in the heel, particularly during movement. Achilles tendonitis involves inflammation of the Achilles tendon, typically causing pain at the back of the heel. A podiatrist offers specialized care for heel pain, providing a thorough evaluation to determine the underlying cause. Treatment options may include custom orthotics, stretching exercises, anti-inflammatory medications, or corticosteroid injections. In severe cases, surgical intervention may be necessary. If you are experiencing heel pain that is interfering with your mobility, it is suggested that you schedule an appointment with a podiatrist for management options.
Many people suffer from bouts of heel pain. For more information, contact Abeer M. Foteh, DPM of Greater Houston Foot Centers. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our office located in Baytown, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Heel Pain
Have you ever gotten up from a chair or out of bed in the morning, and upon taking that first step, feel like your heel has stepped on a tack? Many people experience a feeling of sharp pain which radiates into their arch from their heel and which does not allow them to put their heel on the floor. Sometimes they need to sit back down, stand only on their toes and use the wall for balance. If you can take a few steps, it seems to go away and lessen, allowing you to then resume your activity. Later, throughout your day and after a period of rest, it can happen again. If this sounds familiar you may be suffering from your first attack of heel pain.
Heel pain is a debilitating condition that affects day to day activities. Running and walking both causes stress on the heel because the heel is the part of the foot that hits the ground first. This means that the heel is taking on your entire weight. Diagnosis and treatments for heel pain can be easily found through your podiatrist.
Plantar Fasciitis
One of the main causes of heel pain is a condition known as plantar fasciitis. The plantar fascia is a band of tissue that extends along the bottom of the foot, from the toe to the bottom of the heel. A rip or tear in this ligament can cause inflammation of these tissues, resulting in heel pain. People who do not wear proper fitting shoes are often at risk of developing problems such as plantar fasciitis. Unnecessary stress from ill-fitting shoes, weight change, excessive running, and wearing non-supportive shoes on hard surfaces are all causes of plantar fasciitis.
Achilles Tendonitis
Achilles tendonitis is another cause of heel pain. Similar to plantar fasciitis, inflammation of the Achilles tendon will cause heel pain due to stress fractures and muscle tearing. A lack of flexibility of the ankle and heel is an indicator of Achilles tendonitis. If left untreated, this condition can lead to plantar fasciitis and cause even more pain on your heel.
Heel Spur
A third cause of heel pain is a heel spur. A heel spur occurs when the tissues of the plantar fascia undergo a great deal of stress, leading to a separation of the ligament from the heel bone entirely. This results in a pointed fragment of bone on the ball of the foot, known as a heel spur.
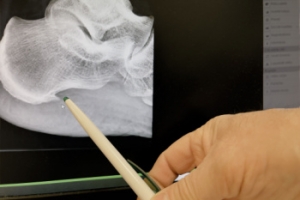
Understanding the Potentially Debilitating Effects of Heel Spurs

Heel spurs, bony protrusions that develop on the underside of the heel bone, can pose significant challenges for individuals affected by this condition. While not always painful, heel spurs have the potential to become debilitating, causing discomfort and limiting mobility. These spurs often result from repetitive strain or stress on the foot, commonly associated with conditions like plantar fasciitis or excessive pronation. As the body attempts to repair itself, calcium deposits accumulate, leading to the formation of a spur. The presence of a heel spur can exacerbate existing foot conditions, causing sharp pain and tenderness, especially during weight-bearing activities such as walking or running. Left untreated, heel spurs may interfere with daily activities and quality of life, impacting overall well-being. Early diagnosis and intervention are vital for managing symptoms and preventing further complications associated with heel spurs. Seeking professional guidance from a podiatrist can help individuals effectively address heel spurs and regain optimal foot health. If you have a heel spur, it is suggested that you are under the care of this type of doctor who can help you manage this condition.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Abeer M. Foteh, DPM from Greater Houston Foot Centers. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in Baytown, TX . We offer the latest in diagnostic and treatment technology to meet your needs.